Osteoporosis vs. Osteoarthritis
Osteoporosis and osteoarthritis often get confused for one another, as they both begin with ‘osteo’; however, they are completely different conditions – you may have only one of them or you may even have them both. Both conditions can cause pain and limit your mobility, but the underlying cause of the pain and mobility restrictions are treated differently. So it is important that you obtain an accurate diagnosis, in order to have a treatment plan that will be successful for you!
| Osteoporosis | Osteoarthritis | |
| Definition | It is a condition that involves the state of your bones. There is a decreased quantity and quality of your bone structure. This can increase your risk of getting a fracture. It affects your overall bone structure. |
It is a condition that involves the state of your joints. There is a thinning and destruction of the cartilage that is normally at the ends of bones. There can also be changes to the bone that lies underneath the cartilage.It affects specific joints. |
| Symptoms | It produces no symptoms, even as the condition progresses. Only when the bone has become weakened to a point that a simple movement (i.e. bending over to pick up something heavy) can cause a fracture, can pain occur. | It produces significant pain that can result in restricted mobility and stiffness. The joints may also appear larger over time, due to an accumulation of fluid in the joint. |
| Risk Factors | Major Risk Factors:
– Low bone mineral density
|
Internal Risk Factors:
– Age External Risk Factors: – Obesity |
| Exercise Therapy | The exercise program would be individualized to the person to include weight-bearing and strength training exercises that can help stop bone loss, maintain/increase bone density, or increase balance and prevent falls. | The exercise program would be individualized to the person to include range of motion and strength training exercises of the muscles surrounding the joint, in order to provide support to the weak and painful joint.If the damage to the joint is severe, a joint replacement surgery may be needed. An exercise program can also be developed in order to prepare yourself for surgery and for recovery after surgery. |
Come into Form & Function to be assessed by one of our healthcare professionals, in order to have a treatment plan developed that will work best for you!
Sonia
Physiotherapy Resident
Exercise for women 60+ …even a little goes a long way!
A recent study in women aged 60-74, showed that exercising even just two times per week (1 aerobic workout and 1 strength training workout) for 16 weeks can improve aerobic fitness and strength, and reduce fat mass. The greatest benefits were seen in women who exercised four times per week (2 aerobic workouts and 2 strength training workouts). Interestingly, benefits decreased when women exercised six times per week (3 aerobic workouts and 3 strength training workouts).
If you’re a woman 60 years or over, use this study as motivation for safe and effective physical activity levels because even a little bit of exercise can make a difference (just don’t overdo it!). Before starting a new exercise program, make sure your health care professional assesses that you are healthy enough to do so. Exercising is an important step to helping improve your health physically and emotionally, so that you can live your life to the fullest.
So women of all ages: let’s keep moving!
Odette Bulaong, ND
Achilles Pain & Weak Glutes
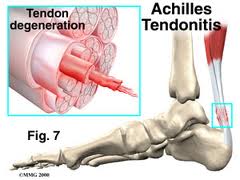
A recent article by Smith et al ( 2013) has shown that runners with Achilles Tendinopathy (chronic tendinitis) also have a delay in both Glute Mede and Glute Max activation and duration of firing. Unfortunately it does not tell us if Glute inactivity is the chicken or the egg, but from a kinetic chain perspective it does make a great deal of sense. Glute Mede and max are external rotators of the leg, and with out good firing patterns, it can also play a part in pronation (foot flattening out) of the foot. Pronation is one mechanism of causing achilles injuries. Either or, if your unsure have your therapist check for glute mede and max response to load, as well as its endurance if you are suffering from Achilles tendon pain.
Neuromotor Control of Gluteal Muscles in Runners with Achilles Tendinopathy
Smith, Melinda M.; Honeywill, Conor; Wyndow, Narelle; Crossley, Kay M.; Creaby, Mark W.
Medicine & Science in Sports & Exercise: 10 October 2013
Choosing the Right Footwear for the Appropriate Sport
Be sure to wear sport-specific shoes when you play a particular sport for at least three times a week. It is highly recommended that you consult with the Chiropodist to ensure that you are wearing the proper shoe size and type of shoe.
The following are just a few shoe recommendations for different types of sports:-
BASKETBALL
Common foot injuries: sprains, tendonitis, stress fractures
The ideal basketball shoe should:
– Have a thick, stiff sole that gives support while running and landing jumps.
– Have a high ankle construction that supports the ankle during quick changes in direction.
SOCCER
Common foot injuries: ankle sprains, turf toe, ingrown toenails
The ideal soccer cleat should:
– Not have more than a half inch of space between your longest toe and the end of the shoe.
– Feature the stud type for the ground that will be played on most often: soft, hard or firm.
TENNIS & BADMINTON
Common foot injuries: ankle sprains, tendonitis, torn knee ligaments
The ideal court shoe should:
– Have a sufficient amount of heel support. Ensure that the area surrounding the heel is stiff enough and
has adequate padding to prevent injury when making quick changes in direction.
– Ensure that the sole of the shoe is stiff to provide support when running.
–
RUNNING
Common foot injuries: plantar fasciitis, shin splints, toenail conditons
The ideal running shoe should:
– Provide maximum shock absorption, to help runners avoid injuries.
– Match your foot’s arch type (low, medium or high)
Choosing the Right Footwear for the Appropriate Sport
Be sure to wear sport-specific shoes when you play a particular sport for at least three times a week. It is highly recommended that you consult with the Chiropodist to ensure that you are wearing the proper shoe size and type of shoe.
The following are just a few shoe recommendations for different types of sports:-
BASKETBALL
Common foot injuries: sprains, tendonitis, stress fractures
The ideal basketball shoe should:
– Have a thick, stiff sole that gives support while running and landing jumps.
– Have a high ankle construction that supports the ankle during quick changes in direction.
SOCCER
Common foot injuries: ankle sprains, turf toe, ingrown toenails
The ideal soccer cleat should:
– Not have more than a half inch of space between your longest toe and the end of the shoe.
– Feature the stud type for the ground that will be played on most often: soft, hard or firm.
TENNIS & BADMINTON
Common foot injuries: ankle sprains, tendonitis, torn knee ligaments
The ideal court shoe should:
– Have a sufficient amount of heel support. Ensure that the area surrounding the heel is stiff enough and
has adequate padding to prevent injury when making quick changes in direction.
– Ensure that the sole of the shoe is stiff to provide support when running.
–
RUNNING
Common foot injuries: plantar fasciitis, shin splints, toenail conditons
The ideal running shoe should:
– Provide maximum shock absorption, to help runners avoid injuries.
– Match your foot’s arch type (low, medium or high)
Measuring Your Physical Activity Intensity
So, you’re jogging on the treadmill, but don’t know if you’re exercising at an appropriate intensity or pace? A way of determining whether you should modify your intensity level is to use the Rating of Perceived Exertion Scale.Using the Rating of Perceived Exertion Scale helps you to determine the efficacy, as well as the safety, of your exercise program. You want to reach a level of intensity that will induce a training effect, while ensuring that you don’t get to a point when you start to experience adverse effects. Heart rate is commonly used, but it can be influenced by many factors, such as certain medications, environmental conditions, and psychological/mood states. The Rating of Perceived Exertion Scale is a reliable alternative to help you self-monitor your exercise intensity on a minute-by-minute basis, allowing you to immediately modify your intensity by speeding up or down your movements.
So, how do you use the scale? The scale ranges from 0 (you are at rest) to 10 (complete exhaustion). When you’re trying to determine what your current level of intensity is, it is important to consider your overall exertion, not just the soreness of a specific body part. Also, since this is a subjective scale, your own appraisal of your exertion is what’s important – don’t compare yourself to other people! As a guide, moderate intensity is considered to be 4-6 on the 0-10 scale and high intensity is considered as 7-9. Discuss your physical activity goals with a healthcare professional at Form and Function to determine at which intensity level you should be training.
The “talk test” is a simpler version of the Rating of Perceived Exertion Scale. If you can sing during your activity, you’re exercising at a low intensity; however, if you can barely get a word out, without having to take a gulp of air, you’re exercising at a vigorous intensity. Therefore, a moderate intensity is when you are exercising, but can still carry on a conversation.
Using this as a starting point, if over time, your rating decreases or you are able to sing while performing the same activity, then you know that your exercise tolerance has improved – great job!
Sonia
Physiotherapy Resident
Measuring Your Physical Activity Intensity
So, you’re jogging on the treadmill, but don’t know if you’re exercising at an appropriate intensity or pace? A way of determining whether you should modify your intensity level is to use the Rating of Perceived Exertion Scale.Using the Rating of Perceived Exertion Scale helps you to determine the efficacy, as well as the safety, of your exercise program. You want to reach a level of intensity that will induce a training effect, while ensuring that you don’t get to a point when you start to experience adverse effects. Heart rate is commonly used, but it can be influenced by many factors, such as certain medications, environmental conditions, and psychological/mood states. The Rating of Perceived Exertion Scale is a reliable alternative to help you self-monitor your exercise intensity on a minute-by-minute basis, allowing you to immediately modify your intensity by speeding up or down your movements.
So, how do you use the scale? The scale ranges from 0 (you are at rest) to 10 (complete exhaustion). When you’re trying to determine what your current level of intensity is, it is important to consider your overall exertion, not just the soreness of a specific body part. Also, since this is a subjective scale, your own appraisal of your exertion is what’s important – don’t compare yourself to other people! As a guide, moderate intensity is considered to be 4-6 on the 0-10 scale and high intensity is considered as 7-9. Discuss your physical activity goals with a healthcare professional at Form and Function to determine at which intensity level you should be training.
The “talk test” is a simpler version of the Rating of Perceived Exertion Scale. If you can sing during your activity, you’re exercising at a low intensity; however, if you can barely get a word out, without having to take a gulp of air, you’re exercising at a vigorous intensity. Therefore, a moderate intensity is when you are exercising, but can still carry on a conversation.
Using this as a starting point, if over time, your rating decreases or you are able to sing while performing the same activity, then you know that your exercise tolerance has improved – great job!
Sonia
Physiotherapy Resident
Natural relief for menstrual cramps
Many women suffer for years from painful periods, a condition known as dysmenorrhea. Fortunately, there are several naturopathic therapies including acupuncture, nutritional changes and herbs that can help provide pain relief.
A study done on 120 females found here, demonstrated that women who consumed ginger root powder for 2 days before their period and the first 3 days of their period experienced less pain and shorter duration of pain than women who did not. Since menstrual cycles are a monthly occurrence, natural therapies such as ginger can be considered by women to decrease their dependence on pain medication.
Remember that in addition to pain relief, naturopathic medicine also helps to determine and treat the cause of painful periods, which is important for female reproductive and overall health.
Odette Bulaong ND
Flexibility vs Mobility
 The best way to think this one through is to imagine “flexibility” as your passive range of motion; it is how far you are able to bend forward . This is usually limited to tonicity of the muscles, tendons, ligaments, fascia, scar tissue and joint capsules.
The best way to think this one through is to imagine “flexibility” as your passive range of motion; it is how far you are able to bend forward . This is usually limited to tonicity of the muscles, tendons, ligaments, fascia, scar tissue and joint capsules.
Mobility on the other hand is how you function within that range of motion. Just because you have good passive range of motion, it does not mean that you are capable of functioning optimally within that range.
Always build mobility as well as flexibility.
