Diabetes and Your Feet

One of the most common complications of diabetes is problems with your feet. In particular, high blood sugars can cause damage to the nerves and the blood vessels in the feet, which can lead to more serious problems such as wounds and amputations. It is important to keep good control of your blood sugars as this can prevent these changes from occurring. If you are diabetic, it is important to have your feet screened yearly to check for any changes.
Contact us to book an appointment today!
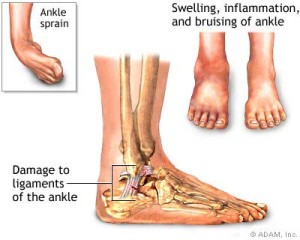
Sprain vs Strain: What’s the difference?
The signs of most sprains or strains are very similar: pain and inflammation, and sometimes bruising, at the injured area. The pain level varies depending on how bad the sprain or strain is. The worse the sprain or strain, the harder it is to use the affected area.The difference is what was stretched or torn to cause the pain.
A sprain is a stretch or tear in a ligament. Ligaments are bands of fibrous tissue that connect bones to bones at joints.
A strain is also a stretch or tear, but it happens in a muscle or a tendon. Tendons link muscles to the bones.
Daily exercise and stretching can prevent sprains and strains. After you get a sprain or strain, it is important to care for the injury by doing proper exercises and stretching as suggested by your health care professional. Please make an appointment with the RMT to discuss what works best for you, your body type, and/or injury.
John Li, RMT
Just because you CAN go doesn’t mean you SHOULD!
Your kidneys are constantly filtering our blood and creating urine which collects in your bladder. Once your bladder is half full, the nerves in your bladder send a signal to your brain and you feel the slight need to urinate. When your bladder is full, another signal is sent and you feel a stronger urge to urinate.This system of signaling between your bladder and your brain keeps your bladder function running smoothly.
If you always urinate before your bladder is full, your bladder ‘learns’ that it cannot hold as much volume as it did before. In other words, you are training your bladder to become smaller. As a result, you may experience the urge to urinate more frequently than before.
So when should you go…? Only when you need to!
Kelly Leong, Registered Physiotherapist
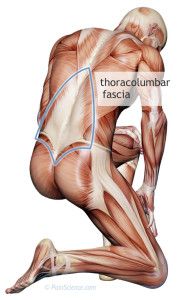
Stretching & Muscle Fascia
Muscle Fascia is the connective tissue that runs throughout your body, between the muscles and the skin. The fascia holds muscles together, keeps each muscle separate so that they can work independently, and allows the muscles to move smoothly against each other. Therefore it is important to keep it well stretched; making it flexible and loose.To allow free movement and to prevent stiffness or tightness, regular stretching and drinking water, will help keep the fascia from seizing up and promotes wider range of motion.
There are many stretching techniques for different parts of your body. Many are fast and easy, so they can be done while waiting in line, at the office, or while watching TV. Please make an appointment with the RMT to discuss what works best for you, your body type, and/or injury.
John Li, Registered Massage Therapist
Shoulder Circles Everyday Keeps Frozen Shoulder Away
The shoulder joint is the most mobile – and thus the least stable – joint in the body. This makes the shoulder a prime candidate to injury during work and during play. Common shoulder injuries include joint capsule sprains, muscular strains, tendinitis, rotator cuff tears, and dislocation. There’s more than meets the eye when talking about the shoulder – many factors often less considered affect the shoulder such as the positioning of the shoulder blade, mid back mobility, and core stability. A great start is doing some Controlled Articular Rotations or CARs each and every morning – Try 7 per arm each and every day to start off your day.Pelvic Health – Let’s talk about it

It’s more common than you think…
1 in 4 women and 1 in 9 men experiences incontinence at some point in their life. Only 1 in 12 cases are known to health care workers because people are often embarrassed to talk about it, or they are afraid health care providers will simply dismiss their symptoms.
7 out of 10 women experience low back pain during pregnancy and 2 out of 10 women experience pelvic girdle pain during pregnancy. Many people are affected by pelvic health dysfunction…so let’s talk about it!
It affects people in different ways…
Our pelvis contains many muscles and other tissues that help to support our organs and joints. These muscles must be able to contract and relax to allow for proper bowel and bladder function, and in women – proper sexual function. We don’t usually pay attention to this system until something isn’t working properly or when symptoms start to appear. Symptoms of pelvic floor dysfunction may include constipation, incontinence, pelvic girdle pain, feelings of ‘heaviness’, painful intercourse or persistent low back pain.
Incontinence is a common symptom in people with pelvic floor dysfunction. Some people experience an extreme urge to urinate but do not experience symptoms of leakage. Some people experience leakage when they cough, sneeze, laugh or jump. Many women also develop low back pain or pelvic girdle pain during pregnancy or after giving birth.
It is often misunderstood…
There are several myths out there about pelvic health and incontinence.
“It is normal to experience urinary leakage after childbirth.”
INCORRECT
Urinary leakage is NOT a normal consequence of childbirth.
“It is normal to experience urinary leakage as you age”
INCORRECT
Urinary leakage is NOT a normal consequence of aging
“Pelvic floor dysfunction only affects women.”
INCORRECT
Pelvic floor dysfunction affects BOTH women and men of all ages.
It impacts your quality of life…
Some people may stop doing certain activities or hobbies because of their symptoms. Many people feel embarrassed so they don’t seek any help. Those dealing with pelvic floor dysfunction may decrease their social activity, physical activity and may become isolated and experience decreased self-esteem. Many people may not seek treatment because they feel that there is nothing that will help.
There IS something you can do about it…
KEGELS ARE NOT ALWAYS THE SOLUTION…
Depending on the type of incontinence you are experiencing, kegels may actually make your symptoms worse! Some types of incontinence may be caused by an overactive pelvic floor.
Doing kegel exercises may cause more overactivity in the pelvic floor and will not help to relieve symptoms.
Your physiotherapist can do a thorough assessment and will give you the correct exercises to either relax or strengthen your pelvic floor. They will also work with you to make sure you are doing the exercises properly and using the correct muscles.
PHYSIOTHERAPY CAN HELP!
Research has shown that pelvic health physiotherapy is effective in treating symptoms of incontinence and should be included in the first line of treatment for urge and stress incontinence (Dumoulin & Hay-Smith, 2010). There is also research to support the use of pelvic floor physiotherapy in treating painful bladder conditions (American Urological Association, 2010).
The Society of Obstetricians and Gynaecologists of Canada also recommends that pelvic floor physiotherapy and core stability training be incorporated to prevent and treat pelvic and back pain during and after pregnancy (Britnell et al., 2005). In France, pelvic floor physiotherapists are involved in pre- and post-partum care for all women. This is not yet the standard of care in Canada.
A proper assessment by a pelvic health physiotherapist will help to identify the root cause of your pelvic dysfunction symptoms. Pelvic health physiotherapists use a combination of internal and external assessment and treatment techniques. These include massage, muscle release techniques, acupuncture, pain education and therapeutic exercise to help patients restore proper pelvic floor function.
Your physiotherapist will work with you to ensure that you are comfortable will all the assessment and treatment techniques being performed.
A pelvic health physiotherapist can also help with other conditions:
Prenatal/post-natal back or pelvic pain
Pelvic organ prolapse
Painful intercourse
Chronic pelvic pain
Dyspareunia (difficult of painful sexual intercourse)
Vaginismus
Vulvodynia
Endometriosis
Interstitial cystitis
Chronic prostatitis
Pelvic health physiotherapy is covered under extended health benefit plans.
Have more questions? Not sure if physiotherapy can help?
Contact Kelly Leong, Physiotherapy Resident at kleong@formfunctionclinic.com